
Contact us
Our team would love to hear from you.
We developed a management system for enhanced medical billing and insurance claim submission and processing.

Our long-term partner, MedScope America Corporation, is a private company that provides Personal Emergency Response Systems (PERS). These alert devices are designed to ensure that at-risk patients can remain safe in the comfort of their homes. By enabling users to access immediate medical assistance, PERS products help decrease hospital readmissions and improve health outcomes.
The client faced challenges, including the absence of a sufficient system for claim processing and billing and fragmented or incomplete patient data. As a part of our collaboration with MedScope, we were asked to create a comprehensive and efficient solution to address these challenges.
MedScope
USA
RCM system
Healthcare
C#, JavaScript, TypeScript, HTML, SQL
EffectiveSoft engineers designed and developed a revenue management system to enable streamlined and efficient claim processing and billing. The system includes two modules—for referring agencies and private customers—and streamlines billing and payment processing. To ensure timely and accurate service payments, the system generates monthly invoices for insurance payers and manages insurance claims.
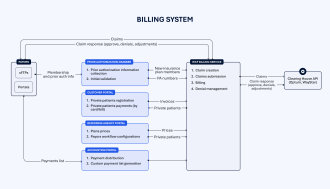
1. Pre-authorization and eligibility checks
At this stage, all relevant information about patients—such as valid address, insurance policy status, coverage limit (if any), AMA and MCO IDs—along with PERS devices and service charges, is collected. Patients’ insurance coverage is validated and invoices are created in electronic or paper format following compliance standards. Claims are generated based on the invoices. This stage helps reduce claim denials and guarantee timely reimbursement.
2. Claim submission
The validated claims are submitted to insurance payers to request reimbursement. The claims are submitted in accordance with payer-specific requirements to minimize the risk of denials. Some claims pass through EZClaim-enabled clearinghouse validation to enhance accuracy.
3. Payment posting
The received payments are matched to claims, and the status of the corresponding invoices is updated. When an invoice is fully paid, it is settled. For overpayments, invoices are settled and deposits for the excess amount are created. In the case of a partial payment, a new invoice is created for the underpaid amount and resubmitted. Denials are handled through denial management.
4. Denial management
Insurance claims can be denied due to inefficient or inaccurate data. In this case, denials are analyzed, corrected, and resubmitted if necessary. This stage helps reduce the number of denials caused by missing or incorrect information.
The system we created offers our client optimized and consistent claim and invoice submission and processing while ensuring compliance with data security standards and regulations.
As our partnership with MedScope continues, our team offers support and assistance in improving the client’s software. For over 10 years, we’ve been helping MedScope’s in-house team enhance their processes and service delivery with new plug-ins, portals, and integrations.
Our team would love to hear from you.
Fill out the form, and we’ve got you covered.
What happens next?
San Diego, California
4445 Eastgate Mall, Suite 200
92121, 1-800-288-9659
San Francisco, California
50 California St #1500
94111, 1-800-288-9659
Pittsburgh, Pennsylvania
One Oxford Centre, 500 Grant St Suite 2900
15219, 1-800-288-9659
Durham, North Carolina
RTP Meridian, 2530 Meridian Pkwy Suite 300
27713, 1-800-288-9659
San Jose, Costa Rica
C. 118B, Trejos Montealegre
10203, 1-800-288-9659